CRANIAL NERVES IN REVIEW
 Updated 5/24
Updated 5/24Opthalmic ( corneal blink reflex).
Maxillary - which supplies the upper jaw
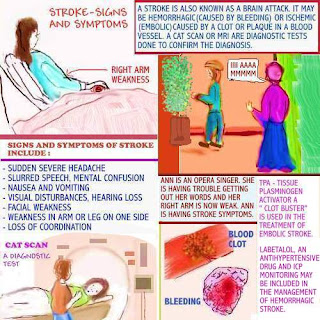
In the image above, Ann is an opera singer.
While on stage, she suddenly starts having
trouble getting her words out. Her right arm
also feels weak. These symptoms are classic
of stroke symptoms.
Severe headache, mental confusion, visual
disturbances and right or left sided weakness
ma occur.
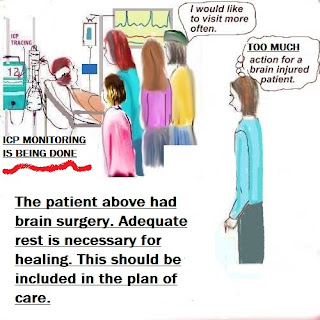
Learn more: The care plan
For more helpful information, please click on the links below:
.JPG)